Imagine this: You’ve just left the dental office, feeling a bit numb but relieved that your oral surgery – perhaps a wisdom tooth extraction or the start of your journey to a new smile with a dental implant placement – is complete. You get home, and suddenly, a crucial question pops into your head: “What on earth can I eat?” It’s a common moment of confusion, and for good reason! What you eat (and don’t eat) after oral surgery isn’t just about comfort; it’s a critical component of your healing process. Think of it as preparing a construction site: you wouldn’t use flimsy materials and skip the blueprints, right? Your body is building new tissue and repairing itself, and it needs the right “construction materials” to do the job efficiently and effectively. At White Tooth Dental, led by Dr. Kristina Pahuta, we believe in a holistic approach to your oral health – understanding that your mouth is an integral part of your overall well-being.
That’s why providing you with comprehensive guidance on nutritional support for your recovery is just as important to us as the procedure itself.
The Unsung Hero of Healing: Why Food is Your Best Medicine
Many people focus solely on pain management and avoiding complications after oral surgery. While those are vital, the power of proper nutrition is often underestimated.

Your body, specifically your mouth, is undergoing significant trauma and needs to repair damaged tissues, fight potential infection, and rebuild bone and gum structures. Read the link between the food you eat and gum health.
This process demands a constant supply of energy, vitamins, minerals, and protein.
Without adequate nutritional support, healing can be delayed, your immune system might weaken, and you could be at a higher risk for complications.
Conversely, providing your body with the right fuel can accelerate healing, reduce swelling, minimize discomfort, and help you bounce back faster. It’s like giving your body a superpower boost for recovery!
What to Expect Right After Surgery
Immediately following your procedure, you’ll likely experience some soreness, swelling, and possibly some minor bleeding.
Your mouth will feel sensitive, and chewing anything solid will be challenging, if not impossible.
This initial phase is all about gentle care and preventing irritation to the surgical site.
The ‘No Straw’ Rule: Your First Golden Guideline
This is perhaps the most crucial piece of advice you’ll hear. DO NOT use a straw after oral surgery, especially following a tooth extraction.
The sucking motion creates negative pressure in your mouth, which can dislodge the blood clot that forms in the extraction socket.
This dislodgment leads to a painful condition called “dry socket” (alveolar osteitis), which not only causes intense pain but also delays healing. Sip your liquids gently from a cup or spoon.
Your Phased Recovery Plate: A Gentle Journey to Solid Foods
Your dietary needs will evolve as you heal.
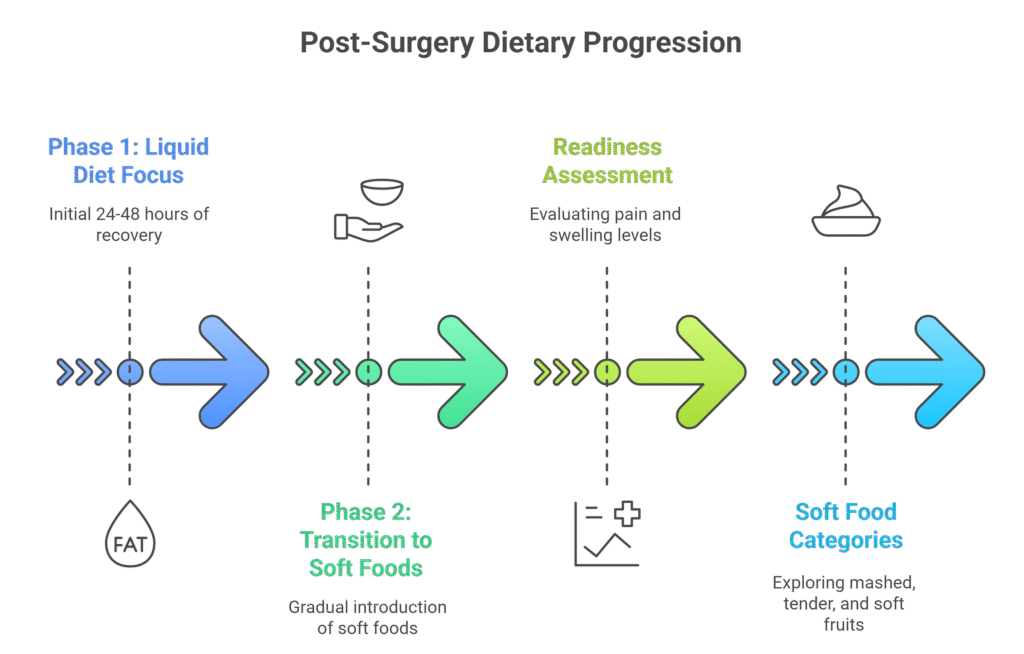
We’ve broken down your recovery into easy-to-understand phases, guiding you from liquids to soft, nutrient-dense meals.
Phase 1: The Immediate Post-Op (Day 1-2) – Liquid Diet Focus
During the first 24-48 hours, stick to a liquid-only or very soft, smooth diet.
The goal here is to nourish without requiring any chewing or irritating the surgical site.
What to Eat (and Drink):
- Cool, Smooth Liquids: Water, clear broths (chicken, beef, vegetable), unsweetened apple sauce, thin yogurt (no fruit chunks), smooth soups (blended cream soups, tomato soup).
- Nutrient-Dense Options: Smoothies made with soft fruits (bananas, berries – strained to remove seeds!), protein powder (unflavored, if tolerated), and liquid bases like milk or plant-based milk.
- Gentle Hydration: Water is your best friend. Staying well-hydrated is crucial for overall cellular function and nutrient transport, aiding your body’s healing processes.
What to AVOID:
- Hot liquids (can increase swelling or dissolve blood clots).
- Alcohol (can interfere with medication and healing).
- Carbonated beverages (bubbles can dislodge clots).
- Spicy or acidic foods/drinks (can irritate the wound).
- Anything that requires chewing.
Phase 2: Transition to Soft Foods (Day 3-7) – Gentle Nourishment
As pain and swelling begin to subside, you can gradually introduce slightly thicker, soft foods. Listen to your body – if something causes pain or discomfort, stop and revert to softer options.
When You’re Ready: You should feel less pain, and swelling should be noticeably reduced.
You might be able to gently open your mouth wider without significant discomfort.
Soft Food Categories:
- Mashed & Pureed: Mashed potatoes (not too hot!), mashed sweet potatoes, pureed vegetables (carrots, green beans), hummus.
- Tender & Easy to Swallow: Scrambled eggs, well-cooked pasta (macaroni, small shells), soft cooked fish (flaky white fish), soft tofu, oatmeal or cream of wheat.
- Soft Fruits: Bananas, avocado, ripe melon (without seeds).
Nutrient Spotlight: Protein – The Body’s Builder
Why is protein so vital?
Think of protein as the primary building block for nearly everything in your body – including new tissues, blood vessels, and collagen, which are all essential for wound healing. It also helps with immune function, protecting you from infection.
Studies, like those published by the National Institutes of Health, consistently emphasize the critical role of adequate protein intake in oral and maxillofacial surgery patients to prevent complications and support recovery.
Soft Food Protein Sources:
- Dairy-based: Yogurt (plain, no fruit chunks), cottage cheese, soft cheeses.
- Eggs: Scrambled, soft-boiled.
- Fish: Flaky, baked, or steamed white fish (cod, tilapia).
- Legumes: Well-cooked and mashed beans (black beans, kidney beans), lentils.
- Smoothies: Add protein powder (whey, pea, soy) or Greek yogurt.
Dispelling the Dairy Myth: Why Your Dentist Might Be Right
One common misconception floating around is that dairy products should be avoided after oral surgery because they can cause phlegm or interfere with healing.
This is largely a myth! For most people, dairy products like yogurt, milk, and soft cheeses are excellent sources of protein, calcium, and probiotics, all of which can support healing and provide easily digestible nutrients.

Unless you have a specific dairy sensitivity, incorporating these into your soft food diet is generally safe and beneficial.
Phase 3: Semi-Solid & Gradual Return (Week 2-4) – Building Strength
As you continue to heal, typically starting around the second week, you can gradually introduce more semi-solid foods. Again, pay close attention to your body’s signals.
Avoid chewing directly on the surgical site.
Advancing Your Diet:
- Soft Meats: Ground chicken or turkey, finely shredded chicken or pork (moist and tender).
- Soft Cooked Vegetables: Steamed broccoli florets, well-cooked carrots, spinach.
- Pasta & Grains: Soft pasta, quinoa, couscous.
- Fruits: Peaches, pears (soft, canned, or cooked).
Nutrient Spotlight: Vitamins A & C, Zinc – The Healing Trio
Beyond protein, specific micronutrients play critical roles in different phases of wound healing and immune response:
- Vitamin C: Essential for collagen synthesis, a key protein for tissue repair and wound closure. It’s also a powerful antioxidant.
- Vitamin A: Important for immune function, cell growth, and vision, contributing to healthy skin and mucous membranes.
- Zinc: Crucial for immune function, cell division, and protein synthesis – all vital for effective wound healing.
Soft Food Sources for These Nutrients:
- Vitamin C: Blended berries (strained), pureed pumpkin or butternut squash, cooked spinach.
- Vitamin A: Mashed sweet potatoes, pureed carrots, soft cooked kale or spinach.
- Zinc: Soft meats (ground beef, chicken), pureed beans, fortified cereals (once chewing is possible), fortified plant-based milks.
Phase 4: Full Recovery (Beyond 4 Weeks) – Long-Term Oral Health
Your dentist will advise you on when it’s safe to return to your normal diet, typically after 4-6 weeks for most common procedures.
Even then, continue to be mindful and gentle around the surgical site for a few more weeks.
Maintaining a balanced diet with plenty of fruits, vegetables, lean proteins, and whole grains is crucial for long-term oral and overall health.
Beyond the Plate: Hydration and Rest
While food is foundational, two other elements are equally critical for a smooth recovery:

- Hydration: We mentioned it earlier, but it bears repeating. Beyond preventing dry socket, adequate water intake supports all metabolic functions, aids in nutrient absorption, and helps your body flush out toxins, all contributing to faster healing. Aim for consistent sips throughout the day.
- Rest: Your body does its best healing when it’s at rest. Avoid strenuous activity and get plenty of sleep. This allows your body to dedicate its energy to repair.
What About Supplements?
While a balanced diet should be your primary source of nutrients, some patients may benefit from specific supplements if their dietary intake is insufficient or if recommended by their dentist.
Always discuss any supplements with your dental team or a healthcare professional before taking them, as some can interact with medications or have other effects.
When to Call Your Dentist
While most post-operative issues are manageable with proper care, it’s essential to know when to seek professional advice.
Contact White Tooth Dental immediately if you experience:
- Severe, persistent pain that doesn’t respond to prescribed pain medication.
- Excessive bleeding that doesn’t stop with pressure.
- Pus or unusual discharge from the surgical site.
- Fever or chills.
- Numbness that doesn’t resolve as expected.
- Difficulty swallowing or breathing.
Our team is always here to provide emergency dentistry when you need us most, and for any concerns you may have throughout your recovery.
Your Questions, Answered: FAQs About Post-Op Nutrition
Q1: How long do I really need to eat soft foods?
A: The duration varies depending on the complexity of your surgery. For a simple wisdom tooth extraction, you might be back to near-normal eating within 7-10 days, but it could be 2-4 weeks or longer for more complex procedures like multiple extractions or dental implant placement. Your dentist will provide specific guidance, but always listen to your body and introduce harder foods gradually.
Q2: Can I eat peanut butter and jelly after oral surgery?
A: Smooth peanut butter (without chunks) and jelly on a very soft bread (like white bread, with crusts removed) or mixed into yogurt or a smoothie can often be introduced in the soft food phase (Phase 2). Avoid crunchy peanut butter, and make sure the bread isn’t sticky or crumbly.
Q3: Are hot dogs okay?
A: Hot dogs are generally not recommended in the early stages. While they might seem soft, they can be rubbery, difficult to chew without proper force, and can contain spices that might irritate the wound. Stick to truly soft, easily mashed foods.
Q4: What about crunchy or chewy foods?
A: Avoid anything crunchy (chips, nuts, popcorn), chewy (steak, tough bread, gummy candies), or sticky (caramel) for at least 2-4 weeks, or until your dentist gives you the green light. These can dislodge blood clots, irritate the surgical site, or get stuck in the wound.
Q5: Can I have coffee?
A: In the immediate post-op period (first 24-48 hours), avoid hot coffee. After that, lukewarm or cold coffee might be okay for some, but be mindful of acidity which can irritate the wound. Black coffee or coffee with milk/cream is generally preferable to highly acidic or sugary coffee drinks. Remember, no straws!
Your Path to a Smooth Recovery
Nourishing your body properly after oral surgery is more than just a recommendation – it’s a proactive step towards a faster, more comfortable recovery.
By understanding what to eat, what to avoid, and why certain nutrients are crucial, you’re empowering yourself to heal optimally. At White Tooth Dental in Toronto, we’re dedicated to providing [comprehensive dental care] that extends beyond your time in the chair. Whether you’re considering [dental implant placement], a [wisdom tooth extraction], or simply looking for preventive care, our team is here to support your oral health journey every step of the way. If you have concerns about dental anxiety, we also offer [sedation dentistry] options to ensure your comfort. For any questions or to learn more about our services, don’t hesitate to reach out. We’re committed to helping you achieve a healthy, confident smile, offering everything from general services to [cosmetic dentistry] solutions tailored to your needs.