Ever wake up with a sore jaw, a dull headache, or even sensitive teeth? You might be experiencing bruxism, more commonly known as teeth grinding or clenching. It’s a surprisingly widespread issue, affecting up to 31% of the population, and while stress often takes the spotlight as the primary culprit, what you eat (and don’t eat!) could be playing a significant, yet often overlooked, role. Imagine your jaw muscles are like a complex orchestra. Sometimes, they’re playing a beautiful, harmonious tune. Other times, they’re wildly out of sync, clenching and grinding without your conscious knowledge, especially at night. This isn’t just uncomfortable; it can lead to serious dental damage, headaches, and even chronic jaw pain. At White Tooth Dental, we believe in a holistic approach to your oral health. This means looking beyond just your teeth and gums to understand how your overall well-being, including your diet, impacts your smile and comfort.
Let’s explore the fascinating connection between your plate and your jaw tension.
Understanding Bruxism: More Than Just a Grin and Bear It Moment
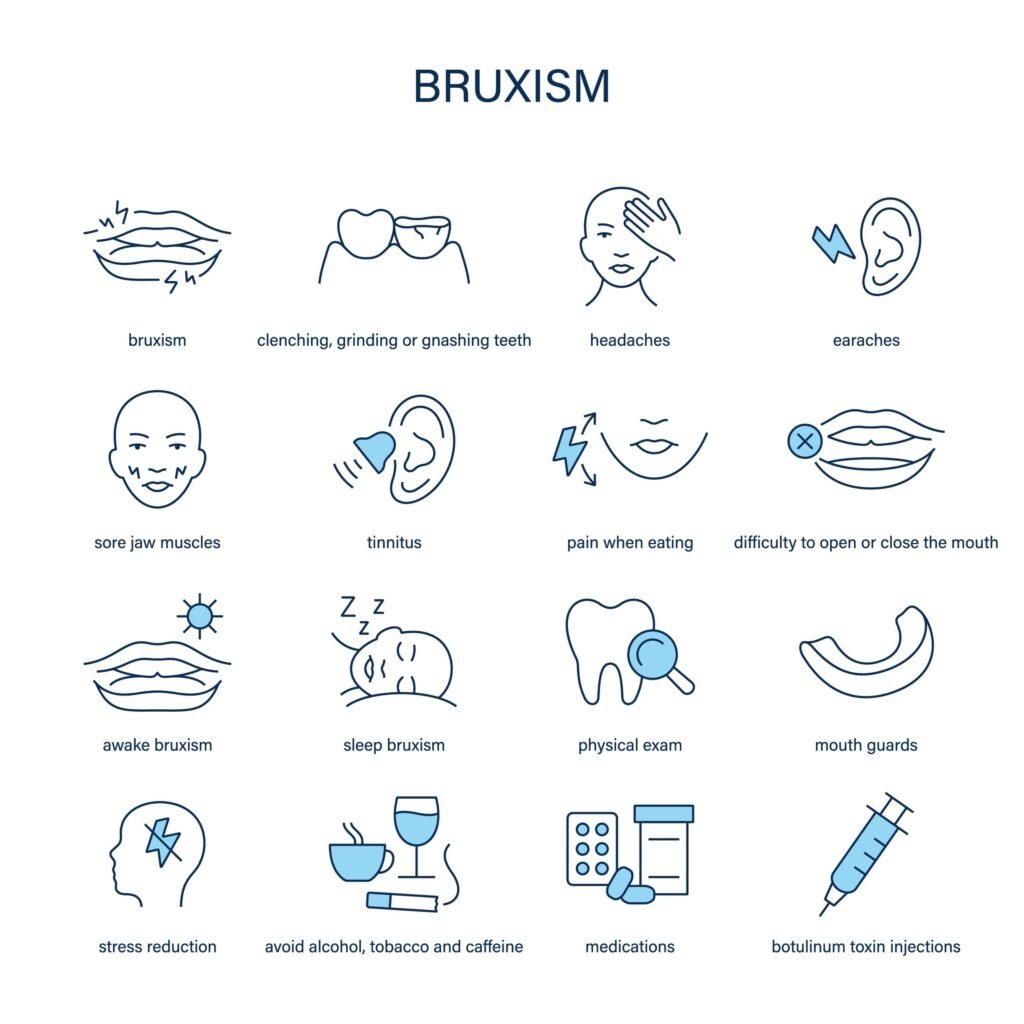
Before we dive into diet, let’s get clear on what bruxism is. It’s the involuntary clenching or grinding of teeth.
It can happen during the day (awake bruxism) or, more commonly, at night while you sleep (sleep bruxism).
Think of your jaw muscles: they’re incredibly strong, designed to bite and chew. But when they’re overused by grinding, they become fatigued and strained, leading to:
- Jaw pain or soreness: Especially in the temporomandibular joints (TMJ), which connect your jaw to your skull.
- Headaches: Often starting in the temples.
- Tooth damage: Worn enamel, chipped teeth, increased sensitivity, and even fractures.
- Facial muscle pain: Can spread to your neck and shoulders.
- Disrupted sleep: For you or your partner, if the grinding is audible.
While stress, anxiety, certain medications, and sleep disorders like sleep apnea are well-known contributors, the role of nutrition is a less-explored but equally impactful piece of the puzzle.
The Surprising Connection: Diet and Your Jaw
You might wonder, “How can my morning coffee or my dinner affect my jaw?”
The link lies in how certain nutrients (or a lack thereof) influence your nervous system, muscle function, and overall inflammation, all of which play a part in jaw tension and bruxism.
The human body is an intricate network.
When certain nutritional building blocks are missing, or when we introduce substances that act as stimulants or inflammatory agents, that intricate network can go awry, sometimes manifesting as muscle tension or restless sleep – prime conditions for bruxism.
Nutrient Power-Up: Filling the Gaps to Calm Your Clench
Our research shows a strong correlation between deficiencies in specific nutrients and the exacerbation of bruxism symptoms.
Think of these as the essential “calming agents” for your muscles and nerves.
Magnesium: The “Muscle Relaxer” Mineral
This is perhaps the most talked-about nutrient when it comes to bruxism, and for good reason!

Magnesium is vital for hundreds of bodily functions, including muscle and nerve function, blood sugar control, and blood pressure regulation.
- How it helps with bruxism: Magnesium acts as a natural muscle relaxant. It helps regulate calcium levels in the body, which is crucial for muscle contraction and relaxation. When magnesium levels are low, muscles can remain in a contracted state, leading to spasms and tension – perfect conditions for jaw clenching. Studies have explored magnesium’s role in alleviating muscle cramps and spasms, which can extend to the jaw muscles.
- Where to find it: Leafy green vegetables (spinach, kale), nuts (almonds, cashews), seeds (pumpkin, chia), legumes (black beans, lentils), whole grains (brown rice, oats), dark chocolate, and avocados.
Vitamin D & Calcium: Bone Health, Muscle & Nerve Synergy
While calcium is essential for strong bones and teeth, it works in tandem with Vitamin D.
Vitamin D helps your body absorb calcium efficiently.
- How they help with bruxism: Both play a crucial role in neuromuscular function. Proper levels ensure that nerve signals are transmitted correctly and muscles contract and relax smoothly. Deficiencies can lead to muscle weakness, cramps, and spasms, potentially contributing to jaw tension. Research has indicated a link between lower Vitamin D levels and bruxism, possibly due to its role in overall muscle health and pain modulation.
- Where to find them:
- Vitamin D: Sunlight exposure, fatty fish (salmon, mackerel), fortified dairy products, egg yolks.
- Calcium: Dairy products (milk, yogurt, cheese), fortified plant-based milks, leafy greens (collard greens, spinach), fortified cereals.
B Vitamins (Especially B5, B12) & Iron: Nerve Support and Energy
The B vitamin complex is a group of eight essential vitamins that play a crucial role in cell metabolism, nerve function, and energy production.
- How they help with bruxism: B vitamins, particularly B5 (pantothenic acid) and B12 (cobalamin), are vital for a healthy nervous system and managing stress responses. B5 supports adrenal function, which is key for stress management, while B12 is crucial for nerve health. Iron, meanwhile, is essential for energy production and can impact fatigue levels, which, when chronic, can exacerbate stress and tension. Some studies suggest a link between B vitamin deficiencies and neurological symptoms that could contribute to bruxism, though the evidence is less direct than for magnesium.
- Where to find them:
- B Vitamins: Whole grains, meat, eggs, dairy, legumes, leafy greens.
- Iron: Red meat, poultry, fish, beans, lentils, spinach, fortified cereals.
Dietary Triggers: What to Watch Out For
Just as some nutrients can help, certain foods and drinks can act as triggers, amplifying jaw tension and grinding.
Hard, Chewy, Crunchy Foods: The Mechanical Strain
This is often an obvious culprit! Constantly chewing on tough foods puts immense strain on your jaw muscles.

- Why they exacerbate bruxism: Think about it: if your jaw muscles are already fatigued from grinding, forcing them to work overtime on a tough steak, a large apple, or a handful of nuts can intensify pain and tension. It’s like asking a tired runner to sprint a marathon.
- Examples: Hard candies, nuts, chewing gum, crusty bread, bagels, tough meats, raw carrots, caramel.
Caffeine & Alcohol: The Stimulants
These are two of the most common dietary culprits for bruxism, as they directly impact your nervous system and sleep quality.
- Why they exacerbate bruxism:
- Caffeine: A stimulant that can increase muscle activity and nervousness, making you more prone to clenching, especially during awake hours. It also disrupts sleep patterns, which can worsen sleep bruxism.
- Alcohol: While it might initially feel relaxing, alcohol disrupts the deeper, restorative stages of sleep (REM sleep). This fragmented sleep can lead to increased muscle activity and grinding during the night.
- Examples: Coffee, tea (especially black and green tea in large amounts), energy drinks, soft drinks, alcoholic beverages.
Sugary & Acidic Foods: Inflammation and Enamel Erosion
While less directly tied to muscle tension, these can contribute to overall oral health issues that exacerbate bruxism symptoms.
- Why they exacerbate bruxism:
- Sugary Foods: Contribute to inflammation in the body. Chronic inflammation can exacerbate pain and muscle tension. They also feed harmful oral bacteria, increasing the risk of cavities, which can be particularly painful if teeth are already sensitive from grinding.
- Acidic Foods: Can erode tooth enamel, making teeth more sensitive and vulnerable to damage from grinding. This erosion combined with grinding makes your teeth feel even more vulnerable.
- Examples: Candies, pastries, sodas, citrus fruits, vinegar, processed foods high in added sugars.
Identifying Food Intolerances/Allergies: A Less Common Link
For some individuals, undiagnosed food sensitivities or allergies could contribute to systemic inflammation and stress responses that might indirectly worsen bruxism.

This is a less common but important consideration for those who have explored other avenues without success.
- When to suspect it: If you experience other unexplained symptoms like digestive issues, skin rashes, or chronic fatigue alongside your bruxism.
- Basic strategy (with caution): An elimination diet, where suspected foods are removed for a period and then reintroduced, can help identify triggers. Always consult a healthcare professional before embarking on restrictive diets.
Bite-Friendly Choices: Fueling a Relaxed Jaw
Now for the good news! Incorporating certain foods can help soothe your jaw muscles and support overall oral health.
Soft Foods for Acute Relief
When your jaw is particularly sore, opting for softer foods can provide immediate relief by reducing mechanical strain.
- Examples: Soups, smoothies, yogurt, mashed potatoes, scrambled eggs, steamed fish, well-cooked pasta, soft fruits (bananas, berries).
- Tip: If you need to include tougher ingredients, try blending them into smoothies or finely chopping them.
Anti-Inflammatory Superfoods: Omega-3s & Antioxidants
Reducing systemic inflammation can have a positive impact on muscle tension and pain throughout the body, including your jaw.
- Omega-3 Fatty Acids: Known for their powerful anti-inflammatory properties.
- Where to find them: Fatty fish (salmon, mackerel, sardines), flaxseeds, chia seeds, walnuts.
- Antioxidants: Combat oxidative stress and inflammation.
- Where to find them: Colorful fruits and vegetables (berries, spinach, broccoli, bell peppers), green tea.
Hydration: Your Jaw’s Best Friend
Staying well-hydrated is fundamental for muscle function and overall health.
Dehydration can lead to muscle cramps and fatigue, potentially worsening jaw tension.
- Tip: Aim for at least 8 glasses of water a day. Keep a water bottle handy as a reminder. Herbal teas (chamomile, peppermint) can also be hydrating and have calming properties.
Beyond the Plate: A Holistic Approach to Jaw Harmony
While diet is a powerful tool, it’s part of a larger picture.
For comprehensive relief from bruxism, we emphasize a holistic approach that integrates lifestyle factors.
Stress Management: The Ultimate Muscle Relaxant
Stress is a major driver of bruxism. Incorporating stress-reducing practices is crucial.

- Techniques: Mindfulness meditation, deep breathing exercises, yoga, spending time in nature, progressive muscle relaxation.
- Impact: These practices help calm your nervous system, reducing the involuntary muscle contractions that lead to grinding. Chronic stress can also deplete essential nutrients, creating a vicious cycle where stress worsens bruxism, and nutrient depletion makes you less resilient to stress.
Sleep Hygiene: The Foundation of Rest
Bruxism often occurs during sleep, so improving your sleep environment and habits can make a significant difference.
- Tips: Maintain a consistent sleep schedule, create a dark and quiet bedroom, avoid screen time before bed, and ensure your diet supports good sleep (e.g., avoiding stimulants like caffeine and alcohol close to bedtime).
- Connection to diet: Nutrient deficiencies (like magnesium) can impact sleep quality, and in turn, poor sleep can exacerbate bruxism.
Jaw Exercises & Physical Therapy
Gentle jaw stretches and exercises can help relax tense muscles and improve jaw mobility.
A physical therapist specializing in TMJ disorders can guide you through appropriate routines.
This might include massage, stretching, and strengthening exercises for your jaw muscles.
When to Seek Professional Guidance
Dietary and lifestyle changes are powerful, but sometimes professional dental or medical intervention is necessary.
- Dental Appliances: A custom-fitted night guard from your dentist can protect your teeth from the damaging effects of grinding while you sleep. This is often the first line of defense recommended by dentists.
- Dental Repair: If your teeth are already damaged from grinding (e.g., chipped, cracked, severely worn), restorative dental procedures may be necessary.
- Botox: In some cases of severe, chronic bruxism, Botox injections into the jaw muscles can temporarily relax them and reduce grinding.
- Behavioral Therapy: Techniques like biofeedback can help you become more aware of clenching habits and learn to relax your jaw.
- Addressing Underlying Issues: If your bruxism is linked to sleep apnea, anxiety, or other medical conditions, a multidisciplinary approach involving a sleep specialist, physician, or therapist may be recommended. For those who experience dental anxiety, our team offers [sedation dentistry options to ensure a comfortable visit.]
At White Tooth Dental, Dr. Kristina Pahuta and our team are here to help you navigate your options and create a personalized plan that addresses your unique needs.
We understand that urgent dental issues can arise from bruxism, and we’re here for emergency dentistry when you need us most.
We also understand the impact bruxism can have on the aesthetics of your smile and can discuss cosmetic dentistry solutions to restore your confidence.
The “Hard vs. Soft Diet” Nuance: A Balanced Perspective

You might have heard that eating soft foods is always best for your jaw. While helpful for acute pain, it’s important to consider the long-term.
Your jawbone, like other bones, needs stimulation to maintain its density and strength.
A diet exclusively of very soft foods over many years can, theoretically, lead to less stimulation of the jawbone, potentially affecting bone health.
The key is balance and awareness. When your jaw is flaring up, prioritize soft foods.
When things are calmer, reintroduce a variety of textures, but chew mindfully and avoid excessive chewing of extremely tough items.
The goal isn’t to never chew anything hard, but to manage the mechanical load on your jaw and ensure your muscles aren’t constantly overworked.
Your Journey to a Calmer Jaw Starts Here
Understanding the link between your diet and bruxism can be a powerful “aha moment.”
It empowers you to take actionable steps towards relief and overall well-being. Remember, small, consistent changes often yield the biggest results.
Here are your practical next steps:
- Start a “Jaw-Friendly” Food Diary: For a week or two, track what you eat and drink, alongside your bruxism symptoms (e.g., jaw pain severity, headaches, morning clenching). This can help you identify your personal triggers and beneficial foods.
- Gradual Dietary Adjustments: Don’t overhaul everything at once. Begin by slowly reducing caffeine and alcohol, incorporating more magnesium-rich foods, and being mindful of very hard or chewy items.
- Prioritize Hydration and Stress Reduction: These are foundational for overall health and directly impact bruxism.
- Talk to Your Dentist: Discuss your symptoms and any dietary changes you’re making. Your dental team can provide insights, check for tooth damage, and recommend appropriate interventions like night guards or further assessments.
At White Tooth Dental, we’re more than just a dental clinic; we’re your partners in comprehensive oral health.
We’re dedicated to educating our Toronto community, fostering a proactive approach to wellness, and making your dental journey comfortable and personalized.
Frequently Asked Questions (FAQs)
Q1: How long does it take to see results from dietary changes for bruxism?
A1: The time frame can vary depending on the individual, the severity of bruxism, and consistency of changes. Some people might notice subtle improvements in jaw tension within a few weeks of consistent dietary and lifestyle adjustments, especially by reducing stimulants and increasing key nutrients like magnesium. Significant, lasting relief usually comes from a combination of diet, stress management, and often, professional dental intervention.
Q2: Can supplements help with bruxism?
A2: Supplements, especially magnesium and Vitamin D, are often considered when dietary intake is insufficient. However, it’s crucial to consult with a healthcare professional (your dentist, doctor, or a registered dietitian) before starting any supplements. They can assess your individual needs, check for potential interactions with medications, and recommend appropriate dosages, as excessive intake of some nutrients can be harmful.
Q3: Is bruxism always caused by diet or stress?
A3: No, bruxism is often multifactorial. While diet and stress are significant contributors, other factors include certain medications (e.g., some antidepressants), sleep disorders (like sleep apnea), genetics, and underlying medical conditions. It’s essential to consider all potential contributing factors for a comprehensive management plan.
Q4: My teeth are already damaged from grinding. Can diet still help?
A4: While diet cannot reverse existing tooth damage, it can play a crucial role in preventing further damage by reducing the severity and frequency of grinding. Additionally, a healthy diet supports overall oral health, which is vital for the longevity of any restorative dental work needed to repair your teeth. Your dentist can help assess the damage and recommend appropriate [restorative dentistry solutions]().
Q5: What’s the best way to get enough magnesium from my diet?
A5: Focus on incorporating a variety of magnesium-rich foods into your daily meals. Great sources include leafy greens (spinach, kale), nuts (almonds, cashews), seeds (pumpkin, chia), legumes (black beans, lentils), whole grains, and dark chocolate. Aim for diverse plant-based foods to ensure a wide range of nutrients.
Q6: If I stop drinking coffee, will my bruxism go away?
A6: Reducing or eliminating caffeine can definitely help, especially if you’re a heavy coffee drinker, as caffeine is a known stimulant that can exacerbate muscle tension and disrupt sleep. However, bruxism is complex. While reducing caffeine is a positive step, it may not be the only solution, and a holistic approach addressing other triggers like stress and nutrient deficiencies will yield the best results.